Welcome to Africa
First, I want to explain my use of the term Africa. Africa is a continent. It is a group of 50-odd countries, most of which were delineated out of convenience for the sake of imperialism. Every country has a far more complex dynamic than that I will ever have the capacity to understand. I visited 4 countries in a limited portion of the continent. I don't have the vocabulary or social awareness to explain every nuance. Therefore, my use of the term Africa is more a matter of convenience than accuracy. An observation made in one place is not necessarily true in another, even in the same part of the same country. More often than not, I found great hope and despair under the same roof.Landing in Livingstone was really what I consider to be the beginning of my time in Africa. While I spent a few days in Cape Town, the lifestyle and urban development, made me feel like I was in Chicago more than I was in Africa, or at least, the image of Africa that most people, myself included, conjure. If not for an utter lack of flights from Peru to Zambia (not as popular route as I had thought), I would have bypassed Cape Town all together.
As it stands, I’m glad I didn’t. Going from one to the other made it easier to compare and contrast the two. Named for one of the first Europeans to explore up the Zambezi River, Livingstone as a town exists for one reason: Victoria Falls, the biggest waterfall (by volume) in the world. While travellers say that Iguazu Falls in Argentina are better overall, there is something serene about standing by what locals know as Mosi au Tunya, or “The smoke that thunders”. And thunder it does. While the Zambia side of the falls all but dry up during the low season (the year round part of the falls is in Zimbabwe), there are some perks of being on the Zambia side. The best side to view the falls is on the Zimbabwe side, but the Zambia side allows you to go up to the VERY edge of Vic Falls. Appropriately, the area is called Devil’s Pool. It is said that this is where Livingstone first stood, completely awestruck, when he first saw the falls. Of course, the locals who actually guided him there have been conveniently forgotten from history and the falls are named for an old hag from England, but I digress.
 |
| Hippos cooling off in the crocodile infested Zambezi River |
 |
| Beautiful |
 |
| Also beautiful |
 |
| The dry Zambia side of the river. In the wet season, this area is under 3 meters of water. |

 |
| Anchoring down because I don't want to fall off and die |
Back to work
After a few days in Livingstone, I headed for Macha Research Trust, a research lab and associated hospital run in partnership with Johns Hopkins Bloomberg School of Public Health. Getting there was certainly an adventure. Macha is in the middle of nowhere. A small town of a few thousand tops, it is located about 6-8 hours from both Livingstone and Lusaka, the capital. There is no direct way to get there. After about 4 hours in the bus, I got off in a relatively large town called Choma. From there, I arranged a taxi to take me the next 1.5 hours on a rocky dusty road to get to Macha.I arrived here not knowing what to expect. Here was this small, unsuspecting town in the middle of rural Zambia and there was novel research happening here? And what about the hospital? The road I had just travelled down had left me feeling a bit like a bobblehead. What about delicate medical or lab equipment? Also, my focus on low resource settings had mostly taken me to urban settings in a more general low resource context. This would add another dimension of challenge for me.
As an example, I am vegetarian. In some parts of Africa, vegetarianism is a somewhat foreign concept. Saying I am vegetarian once resulted in the restaurant serving me chicken along with my vegetables because the idea of abstaining from eating all meat just wasn't fathomable.
Because of the limited and expensive options available in Macha, I had brought almost three weeks of groceries with me. I would be mostly cooking for myself for the duration of the trip. As it is, I enjoy cooking and had had few opportunities to do so during my trip, so this was a blessing in disguise.
 |
| View of Macha from the local watertower |



I was blown away by the team I met at Macha. They are dedicated to making a difference, welcoming, and smart as hell. MRT is engaged in a whole host of activities, with focus particularly on malaria, HIV/AIDS, and TB. Over my time there, I got to survey the range of research interests that the group is focused on.
Before diving into the research, I wanted to understand the context of the place I was working in. Zambia is a rapidly developing country with many layers of complexity, and a long, but feasible, journey ahead. As a disclaimer, it is almost guaranteed that I misheard, misinterpreted, or am not aware of the full context. What I heard, saw, felt, and synthesized are my thoughts on a topic much more nuanced than what I write below.
There are 12-14 tribal groups in Zambia, with 76 dialects spoken. The language of the region is Chitonga, usually simply called Tonga. It is a language with roots tracing back to Bantu. However, English is spoken by many as a result of Christian missionary activity in the region.
The diversity of the country highlights the challenges faced in defining comprehensive public health objectives and strategies. At the same time, efforts undertaken from Macha have made an undeniable impact. Rural births are rarely registered in Zambia, highlighting the difficulty in identifying and responding to areas of need. Malaria cases often are not reported. There is a high prevalence of HIV/AIDS, and mother-to-child transmission remains a challenge.
Infrastructure challenges are present as well. Only 2% of people have piped water and over 50% of people have a non-secure water source. 74% of people do not have secure sanitation. Unfortunately and unsurprisingly, diarrhea, dysentery, and the occasional cholera outbreak continue to affect millions.
In rural areas, medicine is also a spiritual or familial affair. Witch doctors are still commonly recognized for their prodigious ability to heal as well as lift (and place) curses on people. Family feuds can turn into a war of witch doctors, with one family paying large amounts of money to a witch doctor to place a curse on a member of another family, the cursed family paying a bunch of money to another witch doctor to lift the curse, and then subsequently placing another curse on the first family (for even more money). Rinse and repeat.
Just as in every part of the world, there is a great tradition of African medicine influenced by history, religion, and geography. Witch doctors and their practice of providing charms and talismans is just one aspect of medicine, albeit the one most at odds with science. There are also men and women known as bone setters, who well, set bones. How successful they are at that depends greatly, and their failures can lead to years of pain and potentially surgery for what may have been a routine fracture. Herbal treatments are plentiful as well, treating everything from burns and diarrhea to children's fits (mental health awareness has a way to go) and providing a boost in sexual potency. How much of these efforts is successful is beyond my scope. The one important aspect to mention is that the Zambian government requires healers to send all patients with HIV to a government clinic. Basically, if you have malaria, violent diarrhea, broken bones, or wanna curse Trump, then the witch doctor is for you. HIV? No.
HIV/AIDS
The stigma associated with HIV is very real, but stories from Macha serve as critical examples for how to overcome the greatest barrier. MRT traces its root back to missionaries that have been working in the area for over 50 years. Dr. Thuma, the director of MRT, was born and raised in the area. While I didn't get a chance to meet him as he was back at Hopkins, there was no lack of people willing to sing his praises. One such story relates to his efforts to highlight the importance of knowing one's HIV status.Withholding or not knowing this critical information has contributed to the continued increases in HIV-positive rates especially within families between husband and wife (wives) and from mother to child. Fear of being shunned by families, communities, and churches — something that has happened to countless others — keeps people from finding out or seeking out support or antiretroviral treatment. There are estimated to be over a million people who are HIV-positive in Zambia, a country of just 16 million. Coupled with high birth rates, the HIV burden is still increasing, especially in the youngest and largest population cohorts.
These discouraging numbers do not tell the whole story of Macha, however. While the government has backed a number of initiatives across the country to break this stigma, Dr. Thuma sought out the backing of a more powerful entity: the tribal chief and headmen. The importance of tribes cannot be overstated. There still exist rivalries amongst the tribes of Zambia, and intermarriage between certain tribes is rare, even today. In fact, as outsiders, MRT must seek approval of Chief Macha before beginning a new research project.
Dr. Thuma, who has worked his whole life for the betterment of lives in Macha and Zambia, is highly respected. This trust is an outgrowth of the difference made by many of his ideas in the health and economic prospects of those he works for. This relationship is mutually beneficial, as the successful initiatives begun in Macha have resulted in better outcomes than the rest of Zambia, and subsequently led to a nationwide and regional scaling up based on their model.
When Dr. Thuma explained the importance of getting tested and the importance of revealing one's HIV status, he was not met by indifference or scorn. Rather, amongst the presence of all his headman, Chief Macha publicly revealed his own status and urged his headmen to do so as well. Such a forward thinking approach is as much a product of the authentic relationship Dr. Thuma has with the community as it is Chief Macha's recognition of the importance of the challenge at hand. Throughout the region today, there is increased awareness of the role that local leaders play in conjunction with government policies. People (mostly men) like Chief Macha are trusted because they directly govern matters of tangible importance to the everyday lives of their people. People like Dr. Thuma are trusted because they have demonstrated commitment to a community for decades. They speak the language, eat the food, and partake in the joys and struggles of a people. If there has been any takeaway from meeting the people here in Macha, it is that trust is earned through time. It is not bought. You may have the most noble of intentions, but creating change is slow and requires a relationship and buy-in by people.
Regarding HIV management, treatment efforts today are stronger and more streamlined in Macha. People found to be HIV-positive after testing are provided educational and community support and advisers on a voluntary basis. Antiretroviral therapy costs have dropped through a more decentralized structure. People can get medication from any site across Zambia through a national register, as people are quite mobile, especially truckers who have a significantly higher occurrence of HIV. In Macha, this increased awareness has resulted in almost no cases of mother-to-child transmission of HIV since 2010. While the distribution of ART medication is often restricted to larger secondary and tertiary care sites, there are efforts underway to decrease the cost, time, and distance people must travel to receive medicine by equipping more rural health centers (RHCs).
While these approaches sound appealing from a systemic view, there are underlying social factors that influence how successful these strategies can be. Polygamy in rural Zambia is common, with men in some regions having five wives, on average. Families live on homesteads where each wife has her own hut. The wealthier a man (wealth is measured in cattle), the more wives he takes. Use of condoms or other contraceptives as well as family planning is a decision usually made by the man in the relationship, and the answer is almost always no to contraceptives. Infidelity on the part of the husband, while much more common, is normalized or inconceivable, although far more common. Infidelity on the part of the wife is unacceptable and ostracized, although comparatively less common. Because the wife is only supposed to be sexually active with her husband, and because men obviously cannot have HIV, men infected by HIV are often the responsible party for transmitting HIV to their spouses and children.
 |
| Each wife gets a house |
I honestly do not know too much about HIV/AIDS from a public health perspective and did not dedicate as much time and energy as I could have to understanding the challenges, so I'll leave it at that.
Malaria
Most of my time at MRT was focused on working with the team on its malaria research efforts. I cannot do justice to all the dedicated people that are working here, so I will highlight some particularly outstanding aspects and people that I had the fortune of meeting.An aside to provide some context on malaria and some of the jargon I am throwing around
Malaria is caused by the Plasmodium parasite, of which there are multiple species: Falciparum, Malariae, and Vivax are the biggies. Globally, P. Falciparum is the most common malaria parasite followed by P. Vivax. There are others, but you get the idea.
The parasite is transmitted by the female Anopheles mosquito. Again, multiple species of the mosquito exist, and they live in different parts of the world. Some are more effective than others in harboring and transmitting malaria.
The symptoms of malaria tend to come on as a bad fever might. Fever, chills, nausea, body aches, etc. However, severe malaria can cause brain, liver, and kidney damage. Malaria parasites reproduce by targeting red blood cells where they start reproducing, eventually causing your blood cells to burst. Not fun. Kids are particularly susceptible to more severe cases of malaria.
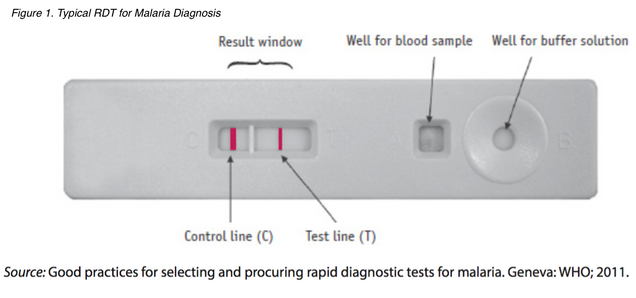
If there is a suspected case of malaria, the most common way to confirm diagnosis is to use a drop of the patient's blood to administer a rapid diagnostic test, or RDT. There are hundreds of millions of RDTs being used around the world. These test are basically structured like pregnancy tests, where a rural community health worker will read the result. These tests (usually) give a positive result if a protein called Histidine-Rich Protein 2, or HRP2, is present. This protein is usually found when the Plasmodium parasite is present.
The standard of care for malaria is Artemisinin Combination Therapy, or ACT. Basically, it is a combination of an older antimalarial with a more recent one called Artemisinin. They are used together to attack the parasite through multiple mechanisms of action and reduce the potential of resistance developing, especially against artemisinin, which is the most effective treatment out there today.
An Overview on Malaria Management in Zambia and Sub-Saharan Africa
Malaria in the district around Macha has declined by an astounding 95% in the past two decades. These astounding reductions are due to a number of measures. If a patient walks into an RHC exhibiting a fever, diarrhea, or other generalized symptoms, their blood is tested using widely available RDTs, or rapid diagnostic tests. Within 30 minutes, RDTs have made it possible to determine whether a patient has a regular fever or malaria. In addition, widespread distribution of bed nets and education campaigns have made a huge difference.
In many of the RHC coverage areas (which can span ~10,000-50,000 people depending on where in Africa you are) in Southern Zambia, as few as 1-2 cases were seen last year. Among the 12-13 centers that work in direct partnership with MRT, there is a robust tracking and GIS modeling system in place. Thus, when there are small patches where malaria spikes, health authorities are able to respond effectively as well as gauge how effective their public health strategy is.
Responses include treatment for the affected (duh), but also a host of other measures that reveal increased understanding about how malaria spreads. It turns out that malaria cases often occur in bunches, both spatially and temporally, especially in regions where malaria has been relatively controlled. The female Anopheles mosquito, the vector for malaria, does not wander far from home, which is usually some body of stagnant water. That means that when one case of malaria pops up, there is a good chance someone close by is at increased risk. As such, there are efforts underway to start educating and/or treating people in proximity of a confirmed case as a prophylactic measure. Of course, this all hinges on people going to RHCs if they suspect they have malaria...overall in Sub-Saharan Africa, the percent of kids with potential symptoms of malaria that were taken to some form of formal health provider was only 47%.
Bed nets are one of the cheapest and most effective preventative measures that can be taken. Just ask the Gates Foundation. Their use has expanded greatly in past years, although there are still people that choose not to use them or do not have them. In recent year, insecticide treated nets, or ITNs, have become the norm, but I saw many people that had older nets than that. Recent numbers from the WHO suggest that 500 million bed nets have been delivered to Sub-Saharan Africa between 2014-16. However, only 50% of homes have sufficient bed nets according to the number of people in their family, and only 54% of at risk people are sleeping under an ITN. While these numbers are for Sub-Saharan Africa at-large, they certainly seemed to reflect reality.
Increasingly, it seemed that people were choosing not to use bed nets, as they are quite stuffy to sleep under (can confirm). Additionally, it is easy to proclaim a public health effort successful in distributing bed nets. However, many of the nets I saw were years old and were ripped in some places. Mosquitoes are sneaky SOBs and if there is anyway they can get in to bite people, they sure as hell will. Getting people nets is important, but they are made of synthetic polyester, not carbon fiber. While distributing 500 million nets is great, how long will those nets last before you need 500 million replacements? In the harsh environment of Sub-Saharan Africa, shit happens.
Couple these efforts with the interesting work being done by the team on the ground, and you can start to understand how research is intricately tied to the evolving public health strategies that have made the region around Macha an effective leader in substantially reducing the burden of malaria.
With the help of Ben, Japhet, Michael, Mukuma, Limonty, Caisan, Bruce, and countless others, I had an amazing time in Zambia working with the team. As a broad overview, I'll highlight what their research looks like.
The team is essentially working on every front of the fight against malaria. When a patient tests positive for malaria, a dried blood spot (DBS) from their finger is transferred to MRT where a battery of tests begins. There is a lot of PCR going on here. For people who have chosen to repress freshman year biology, PCR is short for polymerase chain reaction. If you are looking for something in particular in a sample that is only found in small amounts — like the DNA sequence for a malaria parasite — you can basically target it and cause it to undergo a "chain reaction" to amplify the amount of it. Then, it is easier to find and quantify. Not a perfect definition by any stretch, but hopefully an adequate ELI5.
For patients who test positive for malaria, there are efforts to quantify the type and level of parasite in their blood. One of the things about RDTs is that they are not perfect. RDTs have a lower detection threshold, meaning that they become unreliable or are unable to detect parasite levels of less than a certain amount / volume of blood, often between 50-200 parasites/microliter of blood. However, even having 1 parasite is considered as having malaria. That means that people in the early stages of malaria might not be caught using RDTs. At the same time, there are people that are non-symptomatic. They can inadvertently become reservoirs and lead to other malaria cases. This is a big challenge that public health agencies and RDT producers and researchers are looking at. There are tests that exist with lower detection thresholds, but they cost more. On a large scale, every penny counts. If there are 300 million RDTs produced in the world at the cost of $1.00, that's $300 million. Let's say that the better test cost $1.05. Suddenly, that same money only buys 285 million tests. Per penny, that means 3 million people can or cannot have access to RDTs depending on funding available and quality of test ordered.
That's just one factor to consider. RDTs do not necessarily catch every type of malaria. For example, a patient with P. Vivax malaria would not have a positive result on a test that is designed for P. Falciparum. In Sub-Saharan Africa, P. Falciparum is by far the more prominent malaria, so it isn't as big a deal. However, in Southeast Asia and South America, this can be.
In addition, malaria is evolving. Again, while not a huge problem in Sub-Saharan Africa, malaria is evolving so that it doesn't express the HRP2 antigen. That means that the majority of RDTs on the market would theoretically fail to detect that case of malaria (a false negative). Again, there are efforts to overcome this challenge underway by targeting different proteins associated with the malaria parasite.
After looking at the parasite, the MRT team also looks at the variation in the parasite. Malaria is evolving quickly, and genetic variation of the parasite can lead to some sub-strains of P. Falciparum that may be deadlier, not be as responsive to standard therapy, survive longer in certain conditions, etc. From an epidemiological perspective, such changes can be revealing of changing patterns of disease. If a certain genetic variation becomes increasingly common among malaria-positive patients that doesn't respond the same way to anti-malarials or there is a sudden spike in overall numbers because the parasite's usual life cycle is accelerated (I'm using hypotheticals here), MRT's frontline data allows the country's resources to respond more quickly and efficiently. On a larger scale, tracking the spread of genetic variation from regions where it has been previously documented can allow for preemptive changes in strategy or protocol in accordance with the evolving threat. A prime example is the drug resistant strains of malaria that have appeared in SE Asia. If they suddenly pop up in Sub-Saharan Africa, recognizing it is critical in order to contain and/or manage the situation.

MRT studies the parasite as well as the host. There were a number of different studies going on in that regard. Macha also has a mosquito breeding program and a mosquito house to study the behavior of mosquitoes. The setting allows for controlled studies of what kind of blood meal the mosquitoes prefer, what time of the day they prefer it, where they congregate in a typical house settings, etc.
Bed nets are one of the cheapest and most effective preventative measures that can be taken. Just ask the Gates Foundation. Their use has expanded greatly in past years, although there are still people that choose not to use them or do not have them. In recent year, insecticide treated nets, or ITNs, have become the norm, but I saw many people that had older nets than that. Recent numbers from the WHO suggest that 500 million bed nets have been delivered to Sub-Saharan Africa between 2014-16. However, only 50% of homes have sufficient bed nets according to the number of people in their family, and only 54% of at risk people are sleeping under an ITN. While these numbers are for Sub-Saharan Africa at-large, they certainly seemed to reflect reality.
Increasingly, it seemed that people were choosing not to use bed nets, as they are quite stuffy to sleep under (can confirm). Additionally, it is easy to proclaim a public health effort successful in distributing bed nets. However, many of the nets I saw were years old and were ripped in some places. Mosquitoes are sneaky SOBs and if there is anyway they can get in to bite people, they sure as hell will. Getting people nets is important, but they are made of synthetic polyester, not carbon fiber. While distributing 500 million nets is great, how long will those nets last before you need 500 million replacements? In the harsh environment of Sub-Saharan Africa, shit happens.
Couple these efforts with the interesting work being done by the team on the ground, and you can start to understand how research is intricately tied to the evolving public health strategies that have made the region around Macha an effective leader in substantially reducing the burden of malaria.
Research in Macha
The work at Macha Research Trust is an outgrowth of initiatives from the Bloomberg School of Public Health. Therefore, there is a definite emphasis on parasitology, surveillance, entomology (study of mosquitoes), and using data to improve health outcomes as opposed to biomedical devices. That isn't to say that such work cannot happen. My in at MRT was a Vanderbilt program called VZNIGHT that is working on field testing some new RDTs. |
| The MRT Complex |
With the help of Ben, Japhet, Michael, Mukuma, Limonty, Caisan, Bruce, and countless others, I had an amazing time in Zambia working with the team. As a broad overview, I'll highlight what their research looks like.
 |
| Squad (with some people missing) |
For patients who test positive for malaria, there are efforts to quantify the type and level of parasite in their blood. One of the things about RDTs is that they are not perfect. RDTs have a lower detection threshold, meaning that they become unreliable or are unable to detect parasite levels of less than a certain amount / volume of blood, often between 50-200 parasites/microliter of blood. However, even having 1 parasite is considered as having malaria. That means that people in the early stages of malaria might not be caught using RDTs. At the same time, there are people that are non-symptomatic. They can inadvertently become reservoirs and lead to other malaria cases. This is a big challenge that public health agencies and RDT producers and researchers are looking at. There are tests that exist with lower detection thresholds, but they cost more. On a large scale, every penny counts. If there are 300 million RDTs produced in the world at the cost of $1.00, that's $300 million. Let's say that the better test cost $1.05. Suddenly, that same money only buys 285 million tests. Per penny, that means 3 million people can or cannot have access to RDTs depending on funding available and quality of test ordered.
That's just one factor to consider. RDTs do not necessarily catch every type of malaria. For example, a patient with P. Vivax malaria would not have a positive result on a test that is designed for P. Falciparum. In Sub-Saharan Africa, P. Falciparum is by far the more prominent malaria, so it isn't as big a deal. However, in Southeast Asia and South America, this can be.
In addition, malaria is evolving. Again, while not a huge problem in Sub-Saharan Africa, malaria is evolving so that it doesn't express the HRP2 antigen. That means that the majority of RDTs on the market would theoretically fail to detect that case of malaria (a false negative). Again, there are efforts to overcome this challenge underway by targeting different proteins associated with the malaria parasite.
After looking at the parasite, the MRT team also looks at the variation in the parasite. Malaria is evolving quickly, and genetic variation of the parasite can lead to some sub-strains of P. Falciparum that may be deadlier, not be as responsive to standard therapy, survive longer in certain conditions, etc. From an epidemiological perspective, such changes can be revealing of changing patterns of disease. If a certain genetic variation becomes increasingly common among malaria-positive patients that doesn't respond the same way to anti-malarials or there is a sudden spike in overall numbers because the parasite's usual life cycle is accelerated (I'm using hypotheticals here), MRT's frontline data allows the country's resources to respond more quickly and efficiently. On a larger scale, tracking the spread of genetic variation from regions where it has been previously documented can allow for preemptive changes in strategy or protocol in accordance with the evolving threat. A prime example is the drug resistant strains of malaria that have appeared in SE Asia. If they suddenly pop up in Sub-Saharan Africa, recognizing it is critical in order to contain and/or manage the situation.

 |
| Running gels again... |
MRT studies the parasite as well as the host. There were a number of different studies going on in that regard. Macha also has a mosquito breeding program and a mosquito house to study the behavior of mosquitoes. The setting allows for controlled studies of what kind of blood meal the mosquitoes prefer, what time of the day they prefer it, where they congregate in a typical house settings, etc.
These studies are similarly being conducted in the field. When a case of malaria is found, the team heads over to the site, and as part of its management and treatment program, sets up mosquito traps. The trapped mosquitoes can then be studied to find which mosquitoes are hosts for malaria. Then, the mosquito's DNA is analyzed to correlate what type of Anopheles mosquito each is. Thus, changing patterns of disease can be linked to changing patterns of hosts.
 |
| Limonty and bae (various species of Anopheles mosquitoes) |
 |
| Mosquito house to study mosquito behavior |
 |
| Bruce setting up the mosquito traps as part of fieldwork |
Analyzing the data also allows the team to look to the future. What should malaria management look like down the road? Consider if 200 RDTs were used by a particular RHC and only 2 patients were malaria-positive, it means that theoretically 198 of those RDTs were not necessary. Around Macha, only 2-20% of patients who are suspected of having malaria are positive. Suspicion usually means the patient has a fever. Using regional data, the team is able to ask if there are ways to refine protocol among health workers to more efficiently use RDTs, and thus save money.
Doing Research in the Middle of Nowhere
This was one of my biggest misconceptions with regards to medicine and technology. I thought it hardly happened. While I was certainly humbled in that regard. However, I did learn more about the huge number of considerations that one does not have to make in a lab in the US that one does in rural Zambia. The process of conducting research looks very different because there are different and more constraints.
I already talked about how starting a new study, especially one that may involve the community, requires the approval of a local chief. Couple that with government approval and the headache of bureaucracy and the ethical considerations of any research project and you are off to a strong start.
Consider the space. Maintaining a clean and cool space is an important consideration. Africa is dusty. Loosely, you have a wet and dry season. When it is dry, it is really dry. Dust gets kicked up as you walk around and it hangs in the air. Tainting samples with dust is a general no no. The more apparent challenge is keeping a space cool. Ongoing experiments and reagents that are temperature sensitive can be compromised by higher room temperatures. That requires electricity and an army of air conditioners, which can be unreliable, thus necessitating a backup generator. Don't forget the cost of diesel, which is quite expensive and may not be available in more rural settings! There's also the matter of long term storage of samples. Preserving and storing samples and reagents requires refrigeration at anywhere from 0 to -80 Celsius.
This connects to the issue of procuring equipment and supplies. You can't find -80 freezers in Zambia, or for that matter, most of Africa. Most of it comes used from the States and Europe, an issue I'll talk more about later. I felt like a bobblehead as I was crossing the road from Choma to Macha. Now imagine if I was a carefully calibrated centrifuge or a digital PCR...it would suck to lug out a device worth tens of thousands of dollars only for it to get damaged in transport.
The same holds for things like pipette tips, reagents, lab hoods, and other equipment that is so ubiquitous in Western research institutions. That means when you order something, there's a good chance that it is being shipped from the US, Europe, India, China, or South Africa. (The alternative is that a member of the lab is bringing it personally as part of their own luggage) International orders means international customs. The chance that a Zambian customs agent gives a shit about how your super expensive temperature-sensitive reagent is sitting in the hot and stuffy warehouse is low, and the chance that he'll move any faster because it is time sensitive has to be considered whenever making a purchase.
Research can come to a grinding halt if a necessary reagent isn't available and can only be ordered from thousands of miles away. There isn't another lab down the hall where you can go get some spare PCR reagents. The closest one is hundreds of miles away. The importance of comprehensive knowledge and management of reagents and supplies cannot be overstated. If something is running low, the right person better know and fix it ASAP. This speaks to a frustrating aspect of management in Macha, both with regards to research and the clinic.
If something is running low or you need something ordered, you usually are not empowered to order it. That's fair, as long as the person(s) who are capable individuals. If you need something, it usually involves a lengthy bureaucratic process. You might have to file a request with the procurement office, which is the central office for getting anything by anyone. The maintenance team might want some new mops and you might want a reagent that costs $600. It doesn't necessarily matter. The same person might handle the request. All the requests are aggregated and then what to order is decided. You might have ordered another similar reagent recently, and the procurement team might decide "Hmm...he got some other reagent recently. He's just wasting money. Well, not on my watch. Denied!" If the person working for procurement does not have adequate knowledge of the work done by the research team, things can become a headache quickly.
Alternatively, you might provide all the details and the exact specifications for the filtered 20 microliter pipette tips from Eppendorf that you need. The procurement team might approve it. Then, the finance team gets involved, since they handle all payments. Your perfectly provided URL and specifications somehow gets messed up and you end up receiving the 60-200 microliter size tips or tips from a different company that don't fit with your pipettes! I can feel myself getting a headache just writing about it. The frustration of consistently dealing with the multiple layers of bureaucracy that can derail efforts is real.
I already talked about how starting a new study, especially one that may involve the community, requires the approval of a local chief. Couple that with government approval and the headache of bureaucracy and the ethical considerations of any research project and you are off to a strong start.
Consider the space. Maintaining a clean and cool space is an important consideration. Africa is dusty. Loosely, you have a wet and dry season. When it is dry, it is really dry. Dust gets kicked up as you walk around and it hangs in the air. Tainting samples with dust is a general no no. The more apparent challenge is keeping a space cool. Ongoing experiments and reagents that are temperature sensitive can be compromised by higher room temperatures. That requires electricity and an army of air conditioners, which can be unreliable, thus necessitating a backup generator. Don't forget the cost of diesel, which is quite expensive and may not be available in more rural settings! There's also the matter of long term storage of samples. Preserving and storing samples and reagents requires refrigeration at anywhere from 0 to -80 Celsius.
This connects to the issue of procuring equipment and supplies. You can't find -80 freezers in Zambia, or for that matter, most of Africa. Most of it comes used from the States and Europe, an issue I'll talk more about later. I felt like a bobblehead as I was crossing the road from Choma to Macha. Now imagine if I was a carefully calibrated centrifuge or a digital PCR...it would suck to lug out a device worth tens of thousands of dollars only for it to get damaged in transport.
The same holds for things like pipette tips, reagents, lab hoods, and other equipment that is so ubiquitous in Western research institutions. That means when you order something, there's a good chance that it is being shipped from the US, Europe, India, China, or South Africa. (The alternative is that a member of the lab is bringing it personally as part of their own luggage) International orders means international customs. The chance that a Zambian customs agent gives a shit about how your super expensive temperature-sensitive reagent is sitting in the hot and stuffy warehouse is low, and the chance that he'll move any faster because it is time sensitive has to be considered whenever making a purchase.
Research can come to a grinding halt if a necessary reagent isn't available and can only be ordered from thousands of miles away. There isn't another lab down the hall where you can go get some spare PCR reagents. The closest one is hundreds of miles away. The importance of comprehensive knowledge and management of reagents and supplies cannot be overstated. If something is running low, the right person better know and fix it ASAP. This speaks to a frustrating aspect of management in Macha, both with regards to research and the clinic.
If something is running low or you need something ordered, you usually are not empowered to order it. That's fair, as long as the person(s) who are capable individuals. If you need something, it usually involves a lengthy bureaucratic process. You might have to file a request with the procurement office, which is the central office for getting anything by anyone. The maintenance team might want some new mops and you might want a reagent that costs $600. It doesn't necessarily matter. The same person might handle the request. All the requests are aggregated and then what to order is decided. You might have ordered another similar reagent recently, and the procurement team might decide "Hmm...he got some other reagent recently. He's just wasting money. Well, not on my watch. Denied!" If the person working for procurement does not have adequate knowledge of the work done by the research team, things can become a headache quickly.
Alternatively, you might provide all the details and the exact specifications for the filtered 20 microliter pipette tips from Eppendorf that you need. The procurement team might approve it. Then, the finance team gets involved, since they handle all payments. Your perfectly provided URL and specifications somehow gets messed up and you end up receiving the 60-200 microliter size tips or tips from a different company that don't fit with your pipettes! I can feel myself getting a headache just writing about it. The frustration of consistently dealing with the multiple layers of bureaucracy that can derail efforts is real.
Macha Hospital
Macha Mission Hospital is associated with MRT, and I also had the opportunity to visit the hospital to get a little more clinical insight into the structure of Zambian healthcare overall as well as the resources that a hospital so far from so much has. I've talked a bit about the RHCs already. Theses centers form the primary level of the nation's medical system. They are equipped for the basics. They might only have community health workers or semi-trained health officers, and basically be there as centers to handle HIV and TB patients, identify and treat cases of malaria, and patch up injuries. If a patient has a significant problem, they are sent to a secondary hospital, like Macha. Macha has over 280 beds and can handle most issues, as well as handle surgeries, although there is only 1 surgeon for a catchment area of 150,000 people. In all fairness, there are around 45 for all 16 million people in Zambia so it isn't all that great any way you look at it. I didn't have a chance to talk much with Dr. Spurrier (just as legendary as Dr. Thuma), but he did highlight how doing surgery in such a low resource settings is about doing the best he can do. He is one man doing the job of what should be many more. Finally, patients can be referred to a tertiary hospital. There are very few such hospitals in the country — usually as many big cities are there are, so in the case of Zambia, 2.
Visiting the clinical lab in the hospital, I was impressed at their ability to handle most situations. Most general blood, urine and stool samples and tests can be conducted. One area where I was shocked was with HIV patients. In some cases, patients require certain lab tests to determine the efficacy of ART as well as monitor for abnormalities if the patient has other conditions such as Hepatitis. Because Macha does not have the capacity to monitor patients in such a capacity, they send samples to Lusaka, the capital. It can take up to 6 months to get results back!! The lab technician somberly told me that people often die during this time when their treatment plan is in limbo.
I also had the chance to sit down with one of the only female doctors on staff in Macha. Gender roles in Zambia are slowly evolving, but working in a more rural settings challenged her with patients. Many male patients were unwilling to talk to her, especially if their problems were sexual. In addition, patients often have their own beliefs about what causes certain conditions. As a mother, she had the tenuous role of advocating for the mother of children with disabilities. There is widespread belief that the mother did something wrong when she was pregnant or was unfaithful, leading to this "curse". If a woman was in obstructed labor, a complication that is common in poorer areas among young, malnourished mothers with frequent pregnancies, it suggested that one of the parents had been unfaithful. Going to the hospital when pregnant was a huge step in and off itself. Most deliveries are done by local women who use an eclectic mix of herbs, questionably cleaned razor blades, and in unsanitary conditions. Any complication can be deadly for the mother and child, but the traditional midwife can brush aside responsibility by citing a spiritual reason or curse as the reason for death, not lack of skills or tools.
She also highlighted the lack of basic treatment and diagnosis tools available. When I asked her what tools she wished she had, she laughed and said everything, before settling on an ECG when I pressed her to pick something. The fact that we can sit in class and make ECGs, and here is a hospital that serves 150,000 people that doesn't have enough is shocking, humbling, and maddening.
The challenges, both material and sociocultural, of practicing medicine in a rural setting like Macha highlight why so few doctors stay in rural settings. Doctors are mostly trained in relatively well-equipped modern hospitals. When they are thrust into a setting like Macha, where inadequate resources challenge them to reevaluate their own mindset when trying to treat and diagnose patients, many are unable to handle the pressure or think creatively. It reminded me of Guatemala, where students are continuously rotating through, but rarely returning once they are doctors.
Visiting the clinical lab in the hospital, I was impressed at their ability to handle most situations. Most general blood, urine and stool samples and tests can be conducted. One area where I was shocked was with HIV patients. In some cases, patients require certain lab tests to determine the efficacy of ART as well as monitor for abnormalities if the patient has other conditions such as Hepatitis. Because Macha does not have the capacity to monitor patients in such a capacity, they send samples to Lusaka, the capital. It can take up to 6 months to get results back!! The lab technician somberly told me that people often die during this time when their treatment plan is in limbo.
I also had the chance to sit down with one of the only female doctors on staff in Macha. Gender roles in Zambia are slowly evolving, but working in a more rural settings challenged her with patients. Many male patients were unwilling to talk to her, especially if their problems were sexual. In addition, patients often have their own beliefs about what causes certain conditions. As a mother, she had the tenuous role of advocating for the mother of children with disabilities. There is widespread belief that the mother did something wrong when she was pregnant or was unfaithful, leading to this "curse". If a woman was in obstructed labor, a complication that is common in poorer areas among young, malnourished mothers with frequent pregnancies, it suggested that one of the parents had been unfaithful. Going to the hospital when pregnant was a huge step in and off itself. Most deliveries are done by local women who use an eclectic mix of herbs, questionably cleaned razor blades, and in unsanitary conditions. Any complication can be deadly for the mother and child, but the traditional midwife can brush aside responsibility by citing a spiritual reason or curse as the reason for death, not lack of skills or tools.
She also highlighted the lack of basic treatment and diagnosis tools available. When I asked her what tools she wished she had, she laughed and said everything, before settling on an ECG when I pressed her to pick something. The fact that we can sit in class and make ECGs, and here is a hospital that serves 150,000 people that doesn't have enough is shocking, humbling, and maddening.
The challenges, both material and sociocultural, of practicing medicine in a rural setting like Macha highlight why so few doctors stay in rural settings. Doctors are mostly trained in relatively well-equipped modern hospitals. When they are thrust into a setting like Macha, where inadequate resources challenge them to reevaluate their own mindset when trying to treat and diagnose patients, many are unable to handle the pressure or think creatively. It reminded me of Guatemala, where students are continuously rotating through, but rarely returning once they are doctors.
Fun times
I thought I would be cooking for myself most days. This was a notable exception and a wonderful time with wonderful people. Chris and Marlys Book are amazing. Chris manages operations at Macha and Marlys is one of the sweetest people I've met. She also has a HUGE collection of spices that rivals that of most Indian households, so I was more than glad to cook a meal together with them. It soon grew into a fun-filled team effort. We made chappati, a sweet yogurt dish, Indian daal and baat, and a cabbage sabzi from the fresh vegetables in the Book family garden.
 |
| Domestic |
 |
| And delicious |
 |
| Indian dinner in Macha, Zambia |

No comments:
Post a Comment